Introduction
The uveal tract is highly vascular, and thus accounts for 11% of ocular tumours. These tumours can include:
- Various benign iris nodules and lumps often associated with syndromes or systemic conditions.
- Cysts (stromal, epithelial) represents ~20% of all tumours
- Iris naevi, melanocytoma
- Iris and ciliary body melanoma
- Other rare tumours such as leiomyoma, haemangioma, lung/breast cancer metastasis
Dead Giveaways
Iris Tumours
Small Benign Iris Lesions:
Freckles: Smaller than naevi and occurs at the surface layer only, not stroma
Bruschfield Spots: Pale lesions peripheral iris stroma, often patients with Trisomy 21
Mamillations: Unilateral tiny villiform lesions; uncommon but in patients with congenital ocular melanocytosis, Axenfeld and Peter’s anomaly
Lisch Nodules: Small bilateral nodules after ~16yrs in most Px with NF1

Benign Iris Naevus and Melanocytoma:
Flat (<3mm diameter, <0.5mm thick)
Mostly pigmented, usually no growth → surface proliferation of melanocyte
Typically, melanocytomas are benign lesions formed by melanocytes with dense pigments
May disrupt normal iris structure or distort pupil (ectropion uveae)
Iris and CIliary Body Melanoma:
Uveal melanomas ~3% (cf. ciliary body 10%, choroid 85%)
Often asymptomatic and seen around age ~50-60 years.
Can be diffuse, nodular or sometimes a ring affecting the whole iris
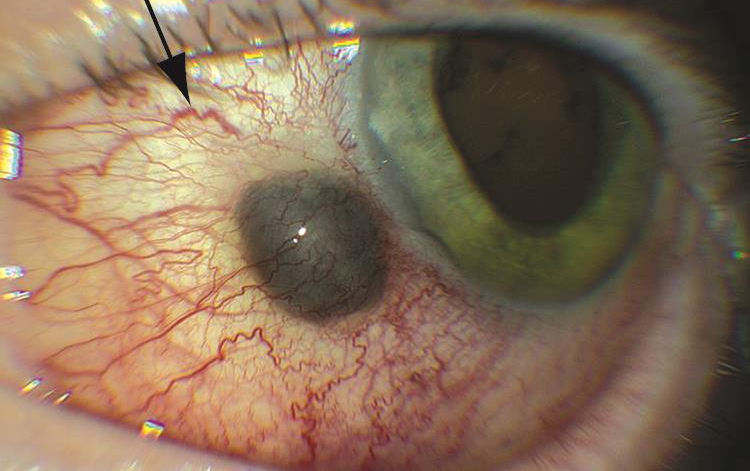
Usually affects the inferior iris, with prominent feeder vessels
Details of the iris are lost, such as the crypts
Can also distort the pupil
Generally, the prognosis is good with only 5% developing metastasis in 10 years

Non-melanocytic Iris Tumours:
Iris vascular tumours like haemangiomas more obvious under OCT-A which reveals tortuous vessels

Iris juvenile xanthogranuloma
Iris lymphoid tumour
Iris metastasis from breast or remote cancer
Iris Pigment Epithelium Adenoma
Rare benign tumour, grey-black nodule with smooth surface, often peripherally, causing anterior displacement and stromal thinning

Ciliary Body Tumours
Ciliary Body Melanoma:
Rare, ~8-10% of uveal melanomas and can often extend to choroid
Very aggressive cf. iris
Good to look for the scleral sentinal vessels or external tumour

Nodule with sentinel scleral vessels Asymptomatic until complications arise, such as glaucoma and VF loss
Detection is fairly late, and prognosis typically poor due to metastatic risk
Other Ciliary Body Tumours:
Leiomyoma = very rare smooth muscle tumour, affecting ciliary body, iris and anterior chamber
Minimal intra/extraocular extension, low mitotic rate
More common in younger women and asymptomatic until it affects nearby structures
Blurred vision, floaters and sometimes pain
Medulloepithelioma = very rare, unilateral embryonic tumour that occurs in first decade
diagnostic features
ABCDEF Grading System: (progression from naevus to melanoma)
A: Age < 40 years
B: Blood or hyphaema
C: Clock Hours Inferior
D: Diffuse
E: Ectropion
F: Feathery Edges
Predisposing factors to melanoma
Fair skin or light iris colour
Cutaneous naevi
Pigmented conditions such as congenital ocular melanocytosis, naevus of Ota, uveal melanocytoma, dysplastic skin melanoma, NF1
UV
Referrals:
Ophthalmologist/ocular oncologist, oculoplastics + pathology, medical oncology
Tx:
Surgical excision, radiotherapy, enucleation for diffuse painful eyes.
Metastatic melanomas: immunotherapy trials.