noso
ommeta
phobia.
An interactive explorer for posterior eye diseases

Case study
Hello!! Welcome to the Posterior Disease section, based on OPTM3205's content. Unfortunately the case-study generator is not online yet, and the first couple lectures have not yet been complete.
It will be ready as soon as possible.
Posterior Eye diseases
Number of Diseases so far
99
Systemic
Diabetic Retinopathy
A systemic condition caused by diabetes which begins to impact the eye.
- Diabetes typically indicated for 11+ mmol/L BSL at random, 7+ mmol/L BSL during fasting
- Is strongly indicated for a HbA1c > 7% on two different tests to allow for irreversible glucose binding
- Longer duration of diabetes increases risk of DR by 6% annually, with a high risk after 10 years
Developmental
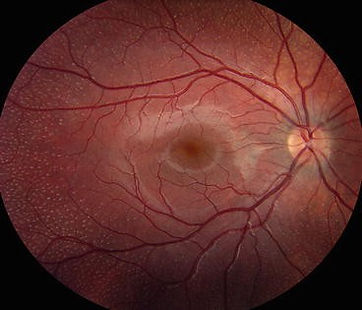
Chorioretinal Coloboma
Caused by the failure of the choroidal fissure to close on day 44, leading to the failed formation of ocular tissue. Whilst it affects the iris, lens, choroid, retina and optic nerve, chorioretinal coloboma affects only the choroid and retina, though can be associated with other colobomas.
Acquired
TIA
A binocular or monocular temporary loss of vision that can be easily missed due to visual input from the non-affected eye compensating for the missing signal. Transient vision loss is only referred to as TIA if neurological dysfunction is caused by a focal brain, spinal cord or retinal ischaemia without infarction.
This means it is not a stroke.
Glaucoma
Primary Open Angle Glaucoma
A group of ocular disorders of multi-factorial aetiology, united by a clinically characteristic optic neuropathy with potentially progressive clinically visible changes at the ONH, comprising focal or generalised thinning of the neuroretinal rim with excavation and enlargement of the optic cup, representing neurodegeneration of the of the retinal ganglion cell axons and deformation of the lamina cribrosa. Corresponding diffuse and localised nerve-fibre-bundle pattern visual field loss may not be detectable in early stages; while VA is initially spared, progression can lead to a full loss.
Posterior Tumours
Optic Nerve Melanocytoma
A melanocytoma is a rare benign lesion located in the optic nerve head, choroid, iris, ciliary body or diffusely in the uvea, conjunctiva or sclera. The ON melanocytoma is thus specifically at the optic nerve, and contains melanocyte sand myelin. This can then extend into the RNFL
Intraocular Lymphoma
PVRL
Primary Vitreoretinal Lymphoma is one of the 3 types of intraocular lymphoma. It is a high grade lymphoma that affects the vitreous body, retina and the optic nerve. These are typically composed of large B-cell lymphomas. VRLs can be secondary, known as DLBCL, or CNS involving or PCNSL.
White Dot Syndrome
APMPPE
Acute Posterior Multifocal Placoid Pigment Epitheliopathy
Typical features include, M = F, 20-30s, bilateral and acute onset, variable viral prodome, Classic WDS symtpoms, resolves in weeks-months, recurrence is rare, multifocal flat gray-white placoid lesions at the level of the posterior pole. RPE improving within 1-2 weeks, and can have disc swelling. Mild vitreous cells, no CNV, good prognosis but can have RPE mottling and depigmentation.
White Dot Syndrome
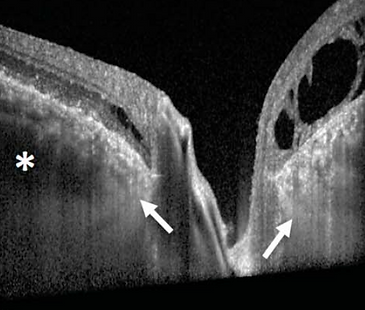
MFC and PIC
Will cover Multifocal Choroiditis and Punctate Inner Choroidopathy
PIC Features: F > M, affects <40years, bilateral, sudden onset, no viral prodome, decreased central VA and WDS. Rare recurrence. Small multiple gray/yellow/opaque round lesions at the level of the RPE-choroid, scattered throughout the posterior pole. Evolves usually into atrophic chorioretinal scars, may be complicated by CNV or subretinal fibrosis. No vitreous cells, 1/3 develop CNV, good prognosis, but scarring and CNV may occur.
MCP Features: F > M, affects 20-60s, bilateral, insidious onset, variable viral prodome, WDS symptoms, chronic duration, recurrency is common, myopic, iritis in 50%, yellow/white lesions whic are replaced by punched out scars. Moderate vitreouc cells, CME may be seen with CNV and generally poor prognosis.
White Dot Syndrome
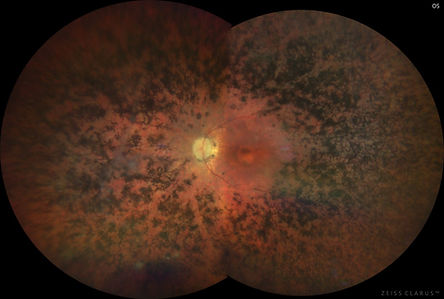
Birdshot Chorioretinopathy
BSC features: primarily affects adult females. Bilateral, with insidious onset and no viral prodome. Classical WDS symptoms but with floaters and difficult night vision, colour vision. Chronic and recurrent. Multiple ill-defined cream lesions at level of outer retina/RPE. Patches of depigmentation, optic atrophy and some disc swelling. Moderate vitreous cells, CME and rare CNV. Guarded prognosis, and strong associateion with HLA-A29.
White Dot Syndrome
Serpiginous Choroidopathy
Predominantly affects males of 30-60s. Bilateral but asymmetrical, with variable onset and no viral prodome. Classical WDS symptoms, but with paracentral scotomas sometimes. Chronic, and recurrent acute lesions last weeks to months. Pseudopodial/geographic zones of gray-yellow discolouration of RPE in peripapillary and macular area with centrifugal extension. Active and peripheral edge at the RPE and choriocapillaris. Vitreous cells can be present or absent, CNV is rare, prognosis is gaurded. Can have RPE mottling, scarring, loss of choriocapillaris and CNV. Associated with HLA-B7, S-antigen.